Legal Update
Feb 21, 2018
Texas and CMS Allow More Expansive Uses of Telemedicine
This is the second in a series of alerts from Seyfarth’s Health Law practice highlighting significant changes in health care regulations and policy as providers and other industry participants enter 2018.
Changes to both federal and Texas law which occurred in 2017 will broaden the circumstances under which physicians can make use of telemedicine services.
In Texas, a bill (SB 1107) which was passed in May 2017 and effective as of September 1, 2017 marks the end of a long and tortured fight between the Texas Medical Board (“TMB”) and Teladoc, a national telehealth provider. Teladoc had waged a years-long campaign against the restrictive Texas telemedicine rules before SB 1107 was signed into law. Prior to the new statute and new rules promulgated by the TMB on September 15, 2017, Texas required an initial face-to-face consultation before a practitioner could utilize telemedicine technology. This seriously limited the effectiveness and potential of telemedicine, particularly in Texas’ rural counties, where physicians and specialists are scarce.
The new law (codified in Chapter 111 of the Texas Occupations Code) allows physicians (or other professionals acting under their supervision) to form a valid practitioner-patient relationship via telemedicine technology, without the need for an initial face-to-face meeting or in-person follow-up visit. Physicians must provide patients with information and guidance about obtaining follow-up care, and with the consent of the patient, provide medical records and other information to the patient’s primary care physician (if applicable). The TMB will require that all services and professionals providing services via telemedicine meet the same standard of care as if performed in an in-person setting. Importantly, under further revisions to the Texas Insurance Code (which were also part of SB 1107), Texas now prohibits insurers from excluding telemedicine services from coverage if the same service would have been covered if performed in-person, as well as any increases to deductibles, copayments or coinsurance for telemedicine services.
The new TMB rules promulgated weeks after SB 1107 went into effect deleted many of the definitions that were key to the more restrictive regulations. The 2017 TMB rules go into greater detail than SB 1107 including on the issue of issuing prescriptions through telemedicine services. As with other types of health care services, the issuance of prescriptions is subject to the same standard of care as a prescription issued after an in-person visit. However, in a nod to concerns about the ongoing opioid crisis, treatment of chronic pain with scheduled drugs via telemedicine is prohibited. The rules likewise emphasize that telemedicine services must meet the same privacy and medical recordkeeping requirements as in-person services, consistent with both Texas and federal law.
CMS, which, like Texas, has also restricted coverage for telemedicine services, introduced new opportunities for telemedicine as part of its bundled care payment models focus on hip and knee replacement surgeries. While participating in these programs, hospitals could utilize telehealth as part of a post-operative plan of care regardless of the patient’s location (including the patient’s home), whereas previously Medicare restricted telemedicine to uses only between two participating facilities. With CMS recently canceling or reducing the scope of certain bundled payment models, it remains to be seen how much these changes will affect the use of covered telemedicine services.
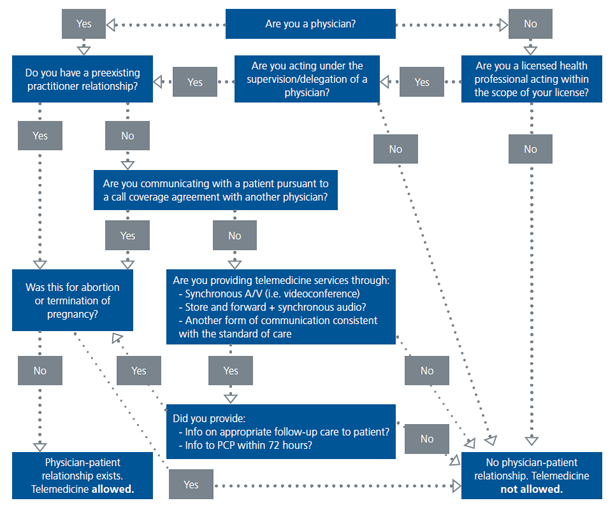
Below is a flowchart showing how and when a physician (or other practitioner) can form a valid practitioner-patient relationship under the new TMB rules.